Ulcerative colitis is a chronic problem that can deeply affect quality of life. It affects millions of people around the world. As one of the two types of inflammatory bowel disease (IBD) it causes inflammation of the colon and rectum.
Let’s understand ulcerative colitis, what are its symptoms, causes and risk factors, along with how it’s diagnosed and treated.
What is Ulcerative Colitis?
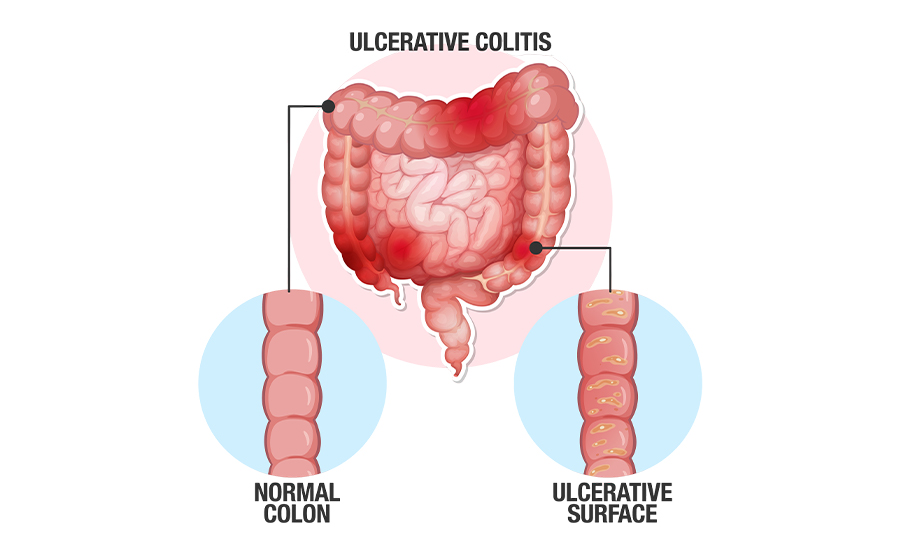
Ulcerative colitis is a type of inflammatory bowel disease (IBD). It causes inflammation and ulcers in the inner lining of the large intestine—called colon—and rectum.
It’s a long term condition and its symptoms usually appear gradually over time, not suddenly.
Symptoms of Ulcerative Colitis
Symptoms of ulcerative colitis vary depending on the severity of inflammation and where it is present.
Common symptoms include:
- Recurrent diarrhoea (may have blood, mucus, or pus)
- Abdominal pain and cramping
- Frequent and sudden (urgent) need to poo
- Not being able to poo despite you feel like you have to (tenesmus)
- Weight loss
- Fever
- Fatigue
- In children: failure to grow
In most people the symptoms are mild to moderate. The course of disease may vary, with some people having long-term periods of remission.
Other Symptoms of Ulcerative Colitis:
Some people who have ulcerative colitis develop conditions and associated symptoms that extend beyond the colon. In such cases, the inflammation can affect other parts of the body such as joints, eyes, skin, and liver.
Possible symptoms include:
- Joint pain and swelling (usually in larger joints like knees, hips, ankles, and wrists)
- Red, irritated, or itchy eyes
- Painful skin rashes or ulcers
- Painful mouth ulcers
Causes of Ulcerative Colitis
The exact cause of ulcerative colitis is not fully known, but some researchers believe that the immune system plays a major role.
Immune System Malfunction:
Normally the immune system protects us by fighting off infections. However, in case of ulcerative colitis, the immune system mistakes the harmless bacteria in your gut as the harmful ones and starts attacking them, causing inflammation in the colon and rectum.
It’s also believed that after fighting off the viral or bacterial infections, the immune system somehow fails to “switch off”. This ongoing immune reaction leads to inflammation in the colon and rectum.
Genetics:
Genetics can also add to the risk of ulcerative colitis. This means having a close relative with ulcerative colitis increases your risk of developing it.
Scientists have identified certain genes connected to the immune system that may make someone more prone to the condition.
Other Risk Factors:
Ulcerative colitis can affect anyone but some factors make it more likely. These include:
Age—usually most people are diagnosed between 15 to 30 years old or later in life after 60.
Race and ethnicity— UC is more common in white people, especially those of Ashkenazi Jewish descent
Family history—having a close relative with ulcerative colitis or Crohn’s disease (the other type of inflammatory bowel disease), raises your risk
Gut microbiome— differences in the balance of bacteria, virus, and fungi in the gut also seems to play a role, although researchers don’t fully understand how
Complications of Ulcerative Colitis
Ulcerative colitis can cause complications like:
- Severe bleeding
- Anemia
- Perforation (a hole) in the colon
- Severe dehydration
- Osteoporosis
- Inflammation of joints, skin, and eyes
- Increased risk of colon cancer
- Toxic megacolon (rapidly swelling colon)
- Increase risk of blood clotting in your veins, arteries, and capillaries
- Delayed growth and development in children
Is Ulcerative Colitis Contagious?
No, ulcerative colitis is not contagious. You cannot spread it or catch it from someone through contact, food, or sharing items. It’s an inflammatory bowel disease, not an infection.
How is Ulcerative Colitis Diagnosed?
To make a diagnosis, your doctor will ask you questions about your symptoms, and medical history.
They’ll also do a physical exam to look for signs like paleness (anemia) or tummy tenderness (inflammation)
They’ll also order some blood tests to check for anemia and inflammation along and a stool sample to rule out infections that may cause similar symptoms
If your doctor suspects ulcerative colitis or crohn’s disease they’ll order further tests like:
- X-ray or CT scan to check for complications
- Sigmoidoscopy—a thin flexible camera tube is used to examine the rectum and lower colon and biopsy samples can also be taken
- Colonoscopy—a camera tube (colonoscope) is used to examine the entire colon. During this examination, biopsy samples can also be taken
Treatment for Ulcerative Colitis
The treatment for ulcerative colitis depends on the severity of your condition and how often your symptoms flare-up.
The main goal of treatment is to control flare-ups (remission) and prevent them from coming back. Treatment usually involves medications and surgery.
Medications:
Doctors use different medications, sometimes in combination, to reduce inflammation, help heal the bowel, and ease symptoms like pain and diarrhoea.
These medications include:
- Aminosalicylates: These are often prescribed for mild to moderate UC (e.g. sulfasalazine and mesalamine)
- Corticosteroids: These are used short-term for flare-ups (e.g. prednisolone). Long-term use can cause side-effects
- Immunosuppressants: They help calm the overactive immune system (e.g. azathioprine and methotrexate)
- Biologics: These target specific parts of immune response for moderate to severe UC (eg. infliximab and adalimumab)
- JAK inhibitors: They’re small-molecule drugs that block certain enzymes involved in triggering inflammation (e.g. tofacitinib)
Surgery:
If medications don’t work or complications develop, surgery may be needed. Around 20% of people with UC need surgery at some point.
There are two types of surgeries:
- Proctocolectomy with ileal pouch: This is the most common procedure for UC. It involves the removal of colon and rectum but leaves the anus. The surgeon creates a new pouch from the small intestine that attaches to your anus. After you heal, it acts as a new rectum allowing normal bowel movements.
- Proctocolectomy with ileostomy: The colon, rectum, and anus are removed. Waste exits through an opening in the abdomen (stoma) into an external pouch that’s emptied regularly
How to Prevent Ulcerative Colitis Flare-Ups?
There’s no guaranteed way to control flare-ups, but you can reduce the risk by avoiding your personal triggers.
Here’s what you can do:
- Manage stress, as it can be one of the triggers for flare-ups
- Avoid use of NSAIDs like ibuprofen, they can make your symptoms worse. Instead of NSAIDs take acetaminophen to relieve pain or fever.
- Avoid your food triggers. Food triggers vary from person to person. But many people find that dairy or high-fiber foods worsen their symptoms. Work with your healthcare provider to make a meal plan for yourself that avoids your triggers but fulfills your nutritional needs.
You can keep a “symptoms and triggers diary”. It can help your doctor understand the pattern of your disease and give you a plan to manage your condition in a better way.
Final Thoughts:
Living with ulcerative colitis can be difficult, but with the right care and support many people manage their symptoms and lead an active life.
If you think you’ve symptoms of ulcerative colitis, don’t hesitate to talk to your doctor. Early detection and management can make a big difference in your quality of life.








